By Haddon Libby
The murder of Brian Thompson of United Healthcare on December 4th may serve as a call to action to reform a badly broken US healthcare system. As a country, we pay just under $12,000 per person for our healthcare. Looking at other countries, Germany is second at $7,400, Canada $5,900, United Kingdom $5,400, Japan $4,700 and South Korea $3,900.
Dr. Dhaval Desai of Emory Saint Joseph’s Hospital in Atlanta said this in a Newsweek article, “This is a rude awakening for everybody that we are in a troubled system where the patient is not always taken care of by the sources that should be taking care of them.”
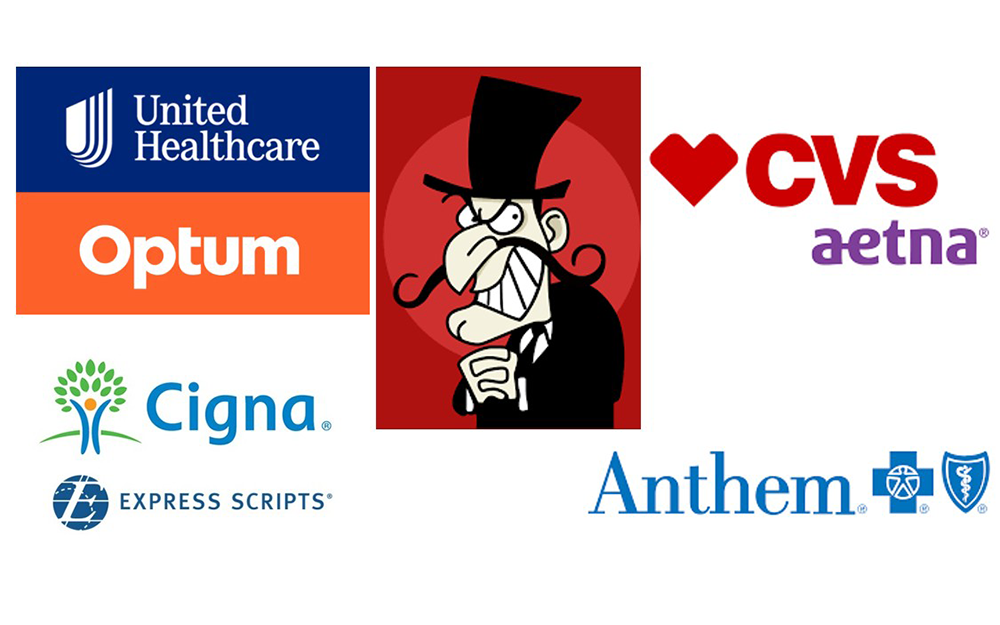
While there are several broken pieces to the healthcare system, insurers and pharmacy benefit managers appear to be the villains. Insurers make more money by delaying and denying medical procedures while three Pharmacy Benefit Managers control 80% of all the pricing of drugs – United Healthcare’s OptumRx, CVS/Aetna and Express Scripts/CIGNA.
Looking at United Healthcare, in-network claims data suggest that this company denies one-third of all claims. Medica is second with a 27% denial rate, Anthem 23%, CareSource and Aetna 20% with Molina at 19% and Cigna at 18%. The industry average is 16%. While these numbers have the potential for error, the industry closely guards its actual denial rates.
Washington DC is likely to make this a hot topic in 2025. Two months before the shooting, the Senate released a report highly critical of CVS/Aetna, Humana and United Healthcare due to sizable increases in claim denials and delays. Sen. Richard Blumenthal, chairman of the US Senate Permanent Subcommittee on Investigations said this, “Insurance companies say that prior authorization is meant to prevent unnecessary medical services. But the Permanent Subcommittee on Investigations has obtained new data and internal documents from the largest Medicare Advantage insurers that discredit these contentions. In fact, despite alarm and criticism in recent years about abuses and excesses, insurers have continued to deny care to vulnerable seniors—simply to make more money. Our Subcommittee even found evidence of insurers expanding this practice in recent years.”
Will Humble, the executive director of the Arizona Public Health Association said, “If insurance companies are not held accountable for their greed, our health care system outcomes will get worse. Across the country, patients can’t afford care, and hospitals can’t afford to keep the lights on and their doors open, while insurers rake in hundreds of billions of dollars. we need more regulation of health insurers to ensure that they are not putting profits before people.”
One of the more disturbing abuses is with a software program called EviCore that UnitedHealthcare and CVS/Aetna use. This software appears to be used to deny or adjust downward claims on Medicare Advantage claims. The problem with EviCore is that it produces bad conclusions in 90% of cases. Insurers state that they do not rely on this AI program for decisions and use it as one of many tools that they use in assessing the legitimacy of claims.
Since the shooting, security measures have increased for senior management of these healthcare providers. At the same time, doctors and nurses are five times more likely to be the targets of violence than other jobs. A poll by the American College of Emergency Physicians reports that nine in ten emergency room doctors have seen violence against them or a colleague in the last year. One in four nurses report abuse in the workplace – mostly by patients. Despite this, senior management in hospitals give employee safety a 4.6 rating on a scale of 1 (low) to 5 (high).
Our best action as users of healthcare is to contact Representative Raul Ruiz and stress the importance of fundamental changes to our healthcare system. He can be reached via his Indio office on Doctor Carreon Blvd, by phone at 760.424.8888 or by visiting ruiz.house.gov.
Haddon Libby is the Founder and Chief Investment Officer of RIA/Fiduciary firm, Winslow Drake Investment Management. www.WinslowDrake.com.